Holistic rehabilitation
The rehabilitation of laryngectomised patients is very complex and includes several subtopics. The first steps of rehabilitation are already taken in the acute clinic. The main aim here is to prepare the person concerned for an independent life in their own home.
Further rehabilitation, such as follow-up treatment, can then be applied for after the stay in hospital. The objectives of the rehabilitation measures are to treat the impairments that arisedue to the illness as well as possible and, in the best case, how to overcome them. In the case of patients who have undergone laryngeal surgery, voice rehabilitation is of great importance. In some cases, the desired objective is also to regain the ability to work and to find one's way back into a working life.
The individual rehabilitation objectives are firmly intertwined and cannot be separated from each other. The individual subtopics are explained in more detail in the following.
Areas of holistic rehabilitation
Rehabilitation of the lung
By removing the larynx, the affected person breathes exclusively through the tracheostoma. The important function of the nose during nasal breathing is thus eliminated. The nose filters, warms and humidifies the respiratory air. These are very important functions which need to be replaced as best possible.
Pulmonary rehabilitation aims to maintain and normalise the function of the lungs and breathing as far as possible to improve physical capacity and thus the quality of life of the person concerned. Frequent pulmonary complications include increased secretion, drying of the mucous membranes in the trachea, a strong and frequent cough, shortness of breath and breathing noises. To counteract these complications, the "artificial nose" or "wet nose" was developed. This is an HME (Heat and Moisture Exchanger) filter that adds heat and moisture to the air when you inhale.
These filters are suitable for all patients, regardless of which substitute voice is being learned. For wearers of a voice prosthesis, there are special filter versions which are closed for speaking with the finger. The HME filters are inserted either into the silicone cannula or into specially designed patch systems. To prevent pulmonary complications in the long term, lung rehabilitation is a crucial part of the measures to improve quality of life.
In speech therapy, specific breathing exercises can be practised for this purpose. Regular inhalation is also crucial for pulmonary health. In addition, physical activity promotes the long-term development of lung volume following laryngectomy.
Smelling and tasting
It is well known that the pleasure of eating is directly related to smelling and tasting. And at the same time, a good nutritional situation is helpful in coping with serious illnesses and promotes the recovery of those affected. Olfactory (smell) and gustatory (taste) rehabilitation are therefore further components of the holistic recovery concept following laryngectomy or tracheotomy.
After surgery, the person no longer breathes through the nose. Smelling is therefore clearly limited at first. However, many nuances of taste are perceived through smell, therefore tasting is also limited. With targeted exercises and rehabilitation measures, it is possible to significantly improve olfactory function again. In speech therapy, various exercises can be practised for this purpose.
The use of an olfactory tube or an olfactory trainer is also often possible. Starting the exercises early is particularly useful here to achieve success quickly. As the loss of the olfactory sense is often perceived as an impairment in quality of life by those affected, it is very important not to neglect this aspect of rehabilitation.
Eating and drinking
Eating is far more than just taking in food. It is pleasure and social togetherness. When we get together with friends or the family, we usually do so to have something to eat together, for example have coffee and cake or share a barbecue.
A healthy person swallows about 2000 times a day. Due to the constant production of saliva, the person has to swallow about once a minute. This happens automatically, without us having to think about it.
After removal of the larynx, the air and food passages are completely separated. Everything that passes through the mouth and is swallowed ends up in the oesophagus and stomach. "Swallowing" in the conventional sense is no longer possible after a laryngectomy for anatomical reasons. The actual swallowing function is only slightly affected by the surgical procedure. However, complications can arise, e.g. from radiotherapy. Here it can well be that saliva production is reduced or food gets stuck at the narrowed entrance to the oesophagus.
Special swallowing techniques can be learned in speech therapy if necessary. Through certain movements and training of the muscles involved, swallowing can be strengthened and food getting stuck can be reduced significantly. Adjusting food consistencies and other adaptive and compensatory measures can quickly lead to success. In case of prolonged difficulties with food intake, a professional nutritionist should definitely be consulted.

Physiotherapy and lymph drainage
Due to the long operation, the altered anatomy, the pain and the resulting relieving posture, affected persons may experience tension and impairment of the musculoskeletal system. In particular, pain can occur in the neck and shoulders. To counteract this, physiotherapy has proved very useful. This can improve mobility and relieve pain through specific exercises. Physiotherapy is also part of holistic rehabilitation and can be prescribed by the physician according to medical findings.
During the surgical removal of the larynx, the lymphatic channels are inevitably severed. Often, the many lymph nodes located in the neck are also removed during laryngectomy by neck dissection to increase the affected person's likelihood of recovery and to avoid a recurrence. Due to this significantly altered anatomical situation, lymphatic congestion often occurs in the tissue. Fluid accumulates between the cells in this process. The skin then appears firm, taut and swollen. This leads to an uncomfortable feeling of tension, can be painful and significantly affects vocal rehabilitation and swallowing as well as the mobility of the tissue region in the neck. Lymphatic drainage is then required and is performed by specially trained physiotherapists. This mobilises the fluid in the tissue to the remaining lymphatic channels where it can then be removed naturally. The tissue becomes softer again and the pain and impairments are noticeably reduced. Lymphatic drainage must be performed regularly. Lymphatic drainage should be started as soon as possible after the completion of clinical treatment. The exact point in time is determined by the ENT physician, also in consultation with the radiotherapist. The physician also issues the prescription for the therapy.
Returning to everyday life
An important component of rehabilitation rests in the hands of those affected themselves. It is crucial to continue participating actively in life despite the changed situation and the serious illness. This includes both participation in social life as well as physical activity. It is conceivable that leisure activities are not feasible to the usual extent, especially shortly after the operation. Nonetheless, it is important not to give up on these and to consistently try pursuing them. Laryngectomised patients can certainly return to work, travel, play sports and attend public events such as concerts. Over time, they learn to trust their body again and to use the possibilities available for coping with everyday situations.
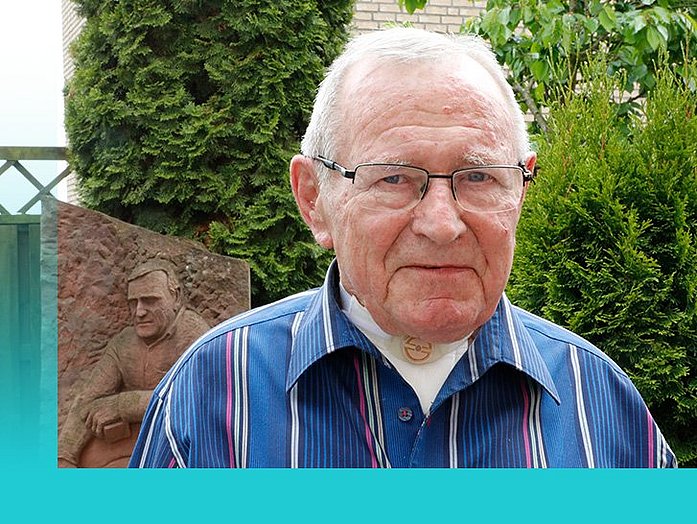
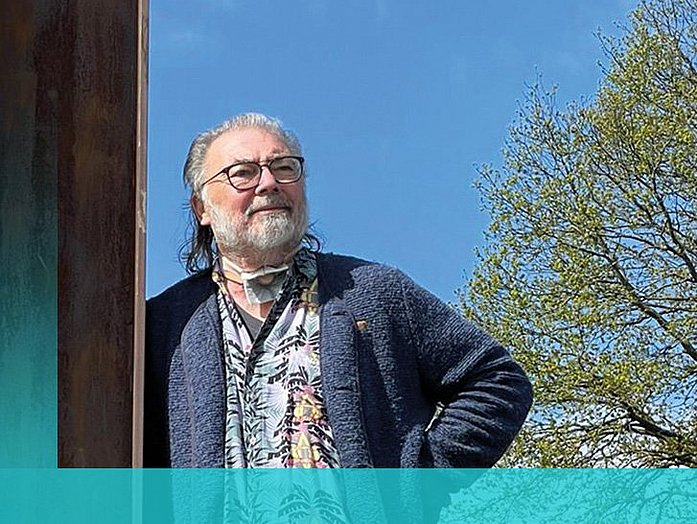
Patient portraits
Examples of the holistic rehabilitation of our patients. Each portrait tells its own experience and provides insight into life with a tracheostoma.