What does the term secretion mean?
In general, secretion is the movement of substances from the cells or glands of our body, which in turn have different tasks for the functioning and maintenance of the organism. This is an automatic process which we cannot actively influence. Although these secretions apparently serve us well, they have tended to be viewed negatively from a societal point of view. It is therefore all the more important in a care situation, to be aware of the significance and generation of these body fluids.
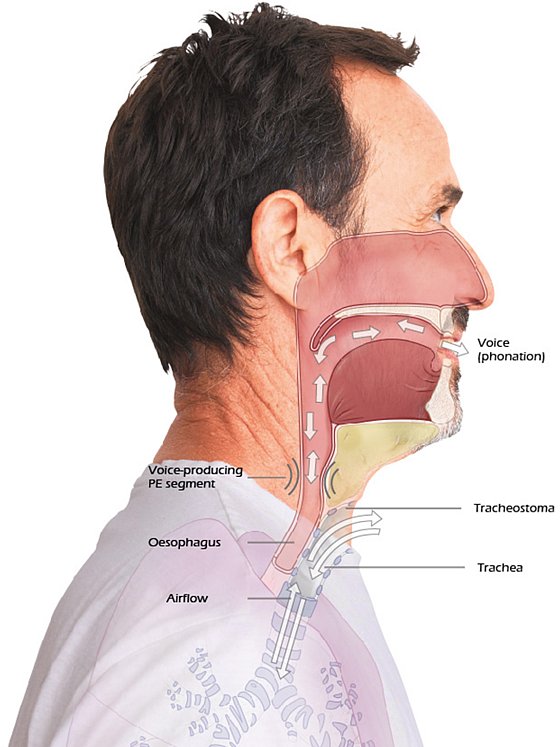
Why do tracheostomy patients have increased secretion?
Next to the loss of nasal function (warming, humidification, filtering), the reason for the often increased formation of secretion lies in the trachea. This is lined with a special structure, the so-called "cilia". These are small hair-like projections which are to prevent the penetration of disease-causing pathogens and particles into the lower airways and the lungs. These are at home in a moist, warm environment and function well.
However, at temperatures below approx. 20-21 degrees and low humidity (<50-55%) they stop functioning. The body reacts spontaneously and largely converts the mucous membrane to secreting goblet cells. As a consequence, this leads to an increased formation of mucus. It is therefore logical, that an unprotected tracheostoma without continuous humidifying and warming measures leads to increased formation of secretion.
Short training course endotracheal Suctioning
In this short training course we explain the basics of endotracheal suctioning.
Are there other triggering factors?
In addition to the functional reasons for increased mucus formation, there are many other promoting factors. The tracheostomy itself already presents a mechanical irritant which triggers secretion. This is particularly the case, if the fit is not perfect in terms of length, curvature or material. Disease-related, e.g. neurological functional disorders may cause pathologically pronounced secretion. In addition, the coughing efficiency of tracheostomised patients is reduced significantly due to the missing vocal fold closure. Thus secretion cannot be drained physiologically and increasingly blocks the airways.

Which measures can be taken
A number of different components play a decisive role in secretion management. First of all, this includes the mobilisation of the secretion through appropriate positioning techniques (VATI) of the patient. Next in line, of course, is the use of technical aids, such as inhalation devices (e.g. HUMIDONEB® NEBULIZER), coughing assistants and of course the endotracheal suctioning. What can provide additional benefits in secretion management?

What additional benefits does secretion management bring me?
In general, one should ensure a good indoor climate with sufficient humidity. Especially during winter months, dry heating air in patients' rooms often leads to increased secretion viscosity (viscous mucus), which can, for example, become apparent through clogging in the tube. Measures for liquefying secretion are therefore paramount.
Inhalations for liquefying secretions have proved highly effective and can be performed with various substances or medicinal products according to the physician's instructions. To avoid possible bacterial transmission and the resulting risk of infection, it is essential to follow the manufacturers' cleaning recommendations for the individual components. Furthermore "Artificial noses“/filters" for inhalation must be removed to prevent excessive humidification with increased breathing resistance.
What effect do artificial noses or wet noses have on increased mucus production?
Often, the efficacy of "Artificial or moist noses" is significantly underestimated. In fact, these filters are extremely well suited for emulating the lost nasal functions. If used consistently over 24h per day, they achieve noticeable re-humidification and warming of the breathing air as well as important filtering. In addition, they generate the necessary breathing resistance which realises complete ventilation of the pulmonary regions. It should be pointed out expressly here, that these filters must be replaced no later than 24h (or immediately if contaminated, i.e. also earlier) to counteract an overshoot in bacterial colonisation. They must definitely not be cleaned as they are designated as single-use items for hygienic reasons.

Subglottic suction with tracheal cannula
The Selection of tracheal tubes can also support secretion management effectively. In case of pronounced secretion, a tube with an inner tube system is recommended. The inner tube can be removed quickly and easily for cleaning if the inner lumen is clogged, whereas the outer tube remains in the tracheostomy. Cleaning of the inner tube is recommended 3x daily and more often if required. If a blocked tube is necessary, then a system with a sub-glottal suctioning option may lead to further positive effects. What is important here, is that the sub-glottal arm should be suctioned intermittently with a syringe. To do this, the patient is to be adjusted to the position of the suction opening above the cuff. This is the only way to effectively suction off the secretion. Despite sub-glottal suctioning, endotracheal suctioning must be performed additionally under all circumstances. Note: a blocked tube offers no absolute protection against aspiration into the lower airways!
And finally, the general fluid balance needs to be mentioned as playing a major role in well functioning secretion management. Far too little attention is often paid to this topic. It is essential for the daily fluid intake to be balanced against the losses due to suctioning, sweating, vomiting, loss of saliva due to difficulties in swallowing,etc., in order to ensure a good fluid balance. The standardised administration of fluids without checking the losses usually does not meet the needs of the patient. Here too, the focus must be on individual and needs-based care.


