Diagnosis laryngeal cancer
The diagnosis "laryngeal cancer" is usually very sudden and unexpected. Your anxieties and worries are now all the greater, as are those of your relatives.
You will already receive considerable information during your first consultation with the treating physician and will be informed about the next steps and the major impending change to your life. It is therefore difficult to remember all the details at first. The surgical opening of a hole in the neck for breathing, the "tracheostoma", and the changed airway are part of the body and will equally place new demands on you, your relatives and caregivers. Everyday things will suddenly have a new significance.
Whereas a tracheotomy merely opens the trachea, a laryngectomy fundamentally changes the anatomy. This is usually caused by advanced laryngeal cancer, which requires a complete surgical removal of the larynx, including the vocal cords and epiglottis.
Due to the resulting elimination of the necessary interface management (safe food intake, breathing, speaking) in the pharynx, a complete separation of the trachea and oesophagus is functionally required to prevent permanent swallowing of saliva and food. Inhalation and exhalation then only take place via the tracheostoma. The upper airways and the important linked functions of humidification, warming and filtering are permanently no longer available. The anatomical changes after a laryngectomy are irreversible and thus make the patient a neck breather for life.
Despite the severity of the clinical picture and the increasing frequency of the disease, especially at a younger age, awareness in our society is still relatively low. Decisive risk factors for the development of laryngeal carcinoma include
- Regular consumption of tobacco
- Alcoholic beverages
- Human Papillomavirus (HPV)
- Specific toxins (poisons)
Is the larynx always removed?
No. Depending on the current findings, the physician in charge will carefully consider whether a complete laryngectomy is absolutely necessary or whether alternative organ-preserving therapies are possible. Certain parameters are of particular importance for the correct decision. In addition to tumour location, the tumour stage and its type, the mobility of the vocal cords is also an important indication for the appropriate choice of therapy. As a result of the treatment, a tracheostoma is usually necessary. This may only be necessary temporarily but, in special cases, also permanently.Depending on the specific tumour, organ-preserving methods such as chemotherapy or antibody therapy, radiotherapy, etc. are further treatment options which are often discussed and coordinated by the attending physicians in consultation with different medical disciplines (tumour board) on a patient-specific basis.
What changes in the field of physiology?
The airways in particular are a very sophisticated body segment. The nasopharygeal cavity offers a particularly large surface area that is completely covered with mucous membrane and occupied by cilia/epithelium. These coordinated structures ensure immediate heating and humidification of the inhaled respiratory air along with filtration of unwanted dirt particles.
Their transport towards the lungs is prevented as best possible by the movement activity of the cilia, and enables elimination of the particles to a large extent by swallowing. The trachea is similarly structured in the lower airways. Over a length of 10 - 12 cm, 16 - 20 horseshoe-shaped cartilage rings provide stability and maintain the necessary inner lumen of the trachea. The system reacts reflexively to the intrusion of foreign bodies by coughing to clear the airways.
The coughing function itself, depends on a necessary build-up of pressure. In a healthy person, this is produced by the closure of the larynx with the epiglottis in combination with the muscle groups responsible for the abdominal press. In both tracheotomised and post-laryngectomy patients, this mechanism is either temporarily or permanently unavailable. Functional limitations are a logical consequence and should be an obligatory consideration in the holistic rehabilitation of these patient groups.
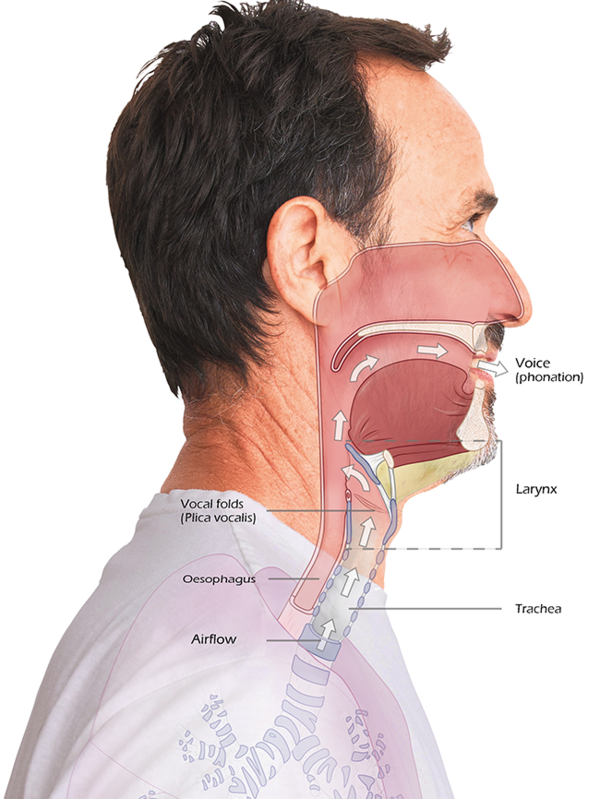
Before the Laryngectomy:
- Larynx present
- Oesophagus and trachea intact
- Interface larynx
- Phonation/Direction/Protection
- Breathing via the mouth, nose throat area
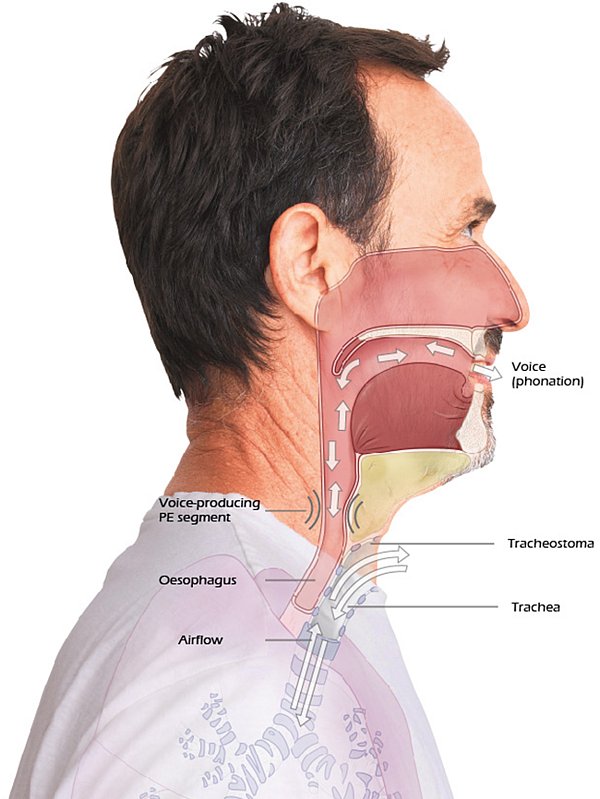
After the Laryngectomy
- Larynx removed
- Trachea and oesophagus separated from each other
- Terminal tracheostoma
- Breathing exclusively via tracheostoma
- Irreversible
The consequences of a laryngectomy
Surgery and the associated changes definitely represent a dramatic change in the patient's life situation. The airway is and remains changed throughout life, chanages from being a mouth/nose breather to a neck breather. This entails special challenges for the personal life situation. Previously unknown aids become necessary and have to be applied or operated.
The consequences of many diagnostic measures of long anaesthesia, radiotherapy and/or chemotherapy sometimes accompany the affected person for a prolonged period of time. Exhaustion and reduced performance up to the fatigue syndrome can follow. It is not uncommon for psychological problems such as lack of drive, isolation in the social and professional sphere, anxiety and even depression to occur. Special complications can also occur at the tracheostoma. Bleeding, infection, granulomas/nodules, stenosis/constriction, shrinkage and scarring have been described.

Loss of nasal function

Risks when taking a shower or bath, and swimming

Limited taste sensation

Primary loss of voice

Separation of trachea
and oesophagus

Less lifting power
Changed airways

Pre- and post-operative
weight loss

Loss of abdominal press

Who falls ill and at what age?
The incidence of laryngeal carcinoma is 2 - 3 times higher in men than in women. However, the incidence of the disease is increasing for female patients. Generally speaking, the risk of developing a tumour increases from the age of 40 onwards. In contrast, a connection between HPV infections and head and neck tumours is more likely to be found in younger population groups.
Typical signs of a head and neck tumour include
- a sore tongue, non-healing mouth ulcers and/or red or white patches in the mouth
- Sore throat
- Persistent hoarseness
- Pain and/or difficulties in swallowing
- Swelling of the neck
- Blocked nose on one side and/or bloody discharge from the nose
What restrictions are to be expected?
The change in anatomy after both tracheotomy and laryngectomy brings with it specific functional losses. Functions that healthy people take for granted, such as voice or smell and taste are no longer present or only temporarily.
It is not uncommon for tracheostoma patients to also experience a significant reduction in performance with an accompanying reduction in quality of life. This makes it all the more important to have rehabilitation measures which are well-tailored to the individual's life situation and enable them to cope with everyday life even under the new conditions.
These measures should be planned and implemented according to the patient's individual resources and needs in order to replace or return the lost functions in the best possible manner. Different rehabilitation options are available for almost every functional loss suffered.

Loss of function and visual change
Attention must also be drawn to the expected visual changes in the external appearance associated with the disease and its therapy. These can be temporary or permanent. Pronounced oedema (swelling) in the facial area is often seen post-operatively, with various tumours in the ear, nose and throat region. Compression bandages in the neck region reinforce this impression. A transnasal probe is usually fixed to the face for a few days following surgery. And of course, the tracheostomy itself often leads to a primary rejection of one's own appearance.
While the tracheotomy often offers the option of a re-transfer, the tracheostoma represents a life-long opening into the trachea in the laryngectomised person. In addition, the neck dissection (on one or both sides), which is occasionally necessary, also leads to a permanently recognisable and significant reduction in neck tissue.


Rehabilitation and medical treatment
The rehabilitation of laryngectomised patients is very complex and includes several subtopics. The first steps of rehabilitation are already taken in the acute clinic. The main aim here is to prepare the person concerned for an independent life in their own home.



